
By Van Ton-Quinlivan, CEO Futuro Health
You don’t have to look further than the daily news headlines to be reminded that we are facing an unprecedented mental health crisis in our nation. The unfortunate aftermath of COVID-19 has resulted in a subsequent pandemic impacting the mental and behavioral health of those in communities across the country, and the numbers are alarming.
According to new data from the National Alliance on Mental Illness (NAMI), one in five adults in America experience a mental illness and nearly one in 25 adults live with a serious mental illness. And, perhaps even more startling, one-half of all chronic mental illness begins by the age of 14. In some instances, this equates to a 25 percent increase in those being diagnosed with behavioral health disorders when compared to pre-pandemic levels.
There have been numerous studies on the pandemic’s impact on the state of mental health in America, many citing isolation, disruptions to schools and businesses, and limitations placed on in-person health care services as contributing factors to the current mental health crisis. While the pandemic was undoubtedly a tipping point in the escalation of mental health diagnoses, behavioral health experts have been warning of looming disruptions for mental health providers for years prior to the repercussions of COVID-19, including job burnout, availability of training, lack of opportunity for minorities, an aging workforce and retirement drain.
These factors become compounded when considering that mental health services have historically been difficult to access in rural communities, where healthcare choices are more limited than they are for residents of cities and suburbia. And for those hoping to find a Black or Spanish-speaking therapist, their options are even less, resulting in significant disparities in care for those who need it most, all of which has only been exacerbated by the aftermath effects of the pandemic.
A Skilled Workforce: Building Blocks to a Solution
It’s difficult to solve the big issues when there are missing pieces to construct the solution. A key piece is always the workforce necessary to do the work. A skilled workforce is one of those building blocks that enables and, when not available, certainly hinders progress.
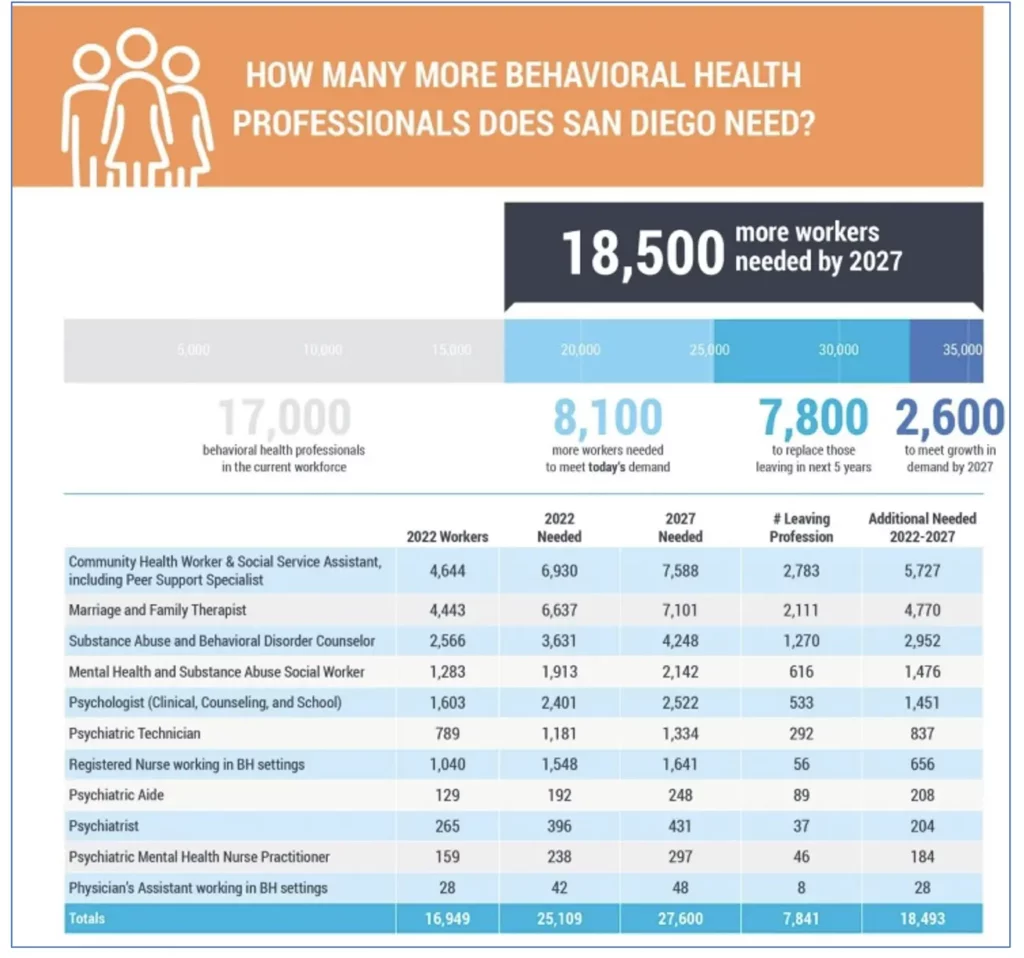
The lack of mental health workers isn’t confined to rural America. In California this week, the San Diego Workforce Partnership issued its own call to action by highlighting the importance of adding more skilled workers as a solution to the mental and behavioral health issues within its own densely populated county lines.
The Workforce’s new report: Addressing San Diego’s Behavioral Health Worker Shortage, emphasizes the need to fill the mental health worker pipeline by educating, training, attracting, employing, and retaining 18,500 additional professionals between 2022 and 2027 to meet the anticipated behavioral health and addiction treatment needs for residents of San Diego County. According to the report, the worker shortage in San Diego County spans a range of titles, some trained through certificates that can be attained under one year, while others require advanced degrees.
Barriers to Mental Health for Racial and Ethnic Minority Groups
Research has shown that racial and ethnic minorities have significantly less access to mental health services than others, and thus are less likely to receive proper care and treatment. Many of these same studies show that one of the best ways to improve health outcomes in underserved communities and among minority populations is to ensure that the medical professionals not only serve their communities but are representative of their communities they serve.
At Futuro Health, we place critical importance in helping students get a tuition-free education in healthcare roles that are in-demand and impactful, filling the gaps caused by differences in income, education, race, ethnicity, and location. Since our launch in 2020, Futuro Health has successfully brought over 8,000 adults back into higher education, with 80% diversity, to train at our partner colleges.
We make education journeys into allied health careers possible by growing the talent that employers need and creating a path to opportunity that workers want.
Investing in Growing the Mental Health Workforce
It is encouraging to see new funding initiatives and legislative actions that many states have taken in response to the need for growing their behavioral health workforce. In California, Gov. Gavin Newsom recently announced a new plan to invest $4.7 billion to overhaul California’s mental health system for children, laying out strategies to improve access to mental health and substance abuse services, including adding 40,000 new skilled workers in mental health fields. This investment comes at a critical time for parents of adolescents experiencing mental health concerns. Since the pandemic the wait time to see a professional has increased to nearly four months according to data from the Association for Behavioral Healthcare.
“Mental and behavioral health is one of the greatest challenges of our time. California is doubling down with the most significant overhaul of our mental health system in state history.”
- California Governor Gavin Newsom
The Governor’s announcement adds to California’s mental health assistance coffers, which includes more than $260 million already earmarked in the state’s 2022-23 budget for initiatives and programs to address the state’s behavioral health crisis. As the Council Vice-Chair of the Health Workforce Education and Training Council – the state’s entity responsible for helping coordinate California’s health workforce education – I foresee these funds creating new and innovative approaches to increase the capacity and diversity of the behavioral health workforce in California over the next one to three years.
The allocation of additional mental health funding comes on the heels of the passage of Senate Bill 803 (SB 803), positioning California on the list of other states that allow certification of Peer Support Specialists, to fill the needed gap in the behavioral healthcare workforce, and improve access, recovery, and outcomes for patients. Peer Support Specialists have lived experience with the process of recovery from mental health or substance use challenges and provide peer support for others experiencing similar issues.
As mental healthcare providers in California prepare for this new benefit, data from other states where Peer Support Specialists have existed for years has proven that professionalizing these roles has bolstered the ranks of mental health workers by providing new pipelines into behavioral health careers for many more individuals seeking jobs in the mental health field. Futuro Health is proud to have been selected as a state approved Medi-Cal Peer Support Specialist Training Program provider, and will begin student enrollment in the program beginning in the fall of 2022.
This is a pivotal time for mental health care providers, educators, workers, and residents of communities everywhere, both large and small. Like other crisis situations, it is vitally important that we approach the mental health workforce shortage crisis in a comprehensive, strategic manner – creating a systems solution, understanding the causes and factors that contributed to the shortage, while keeping focused on actions needed now to recruit and train behavioral workers and get more individuals into the education and training pipeline to fill the vacancies that currently exist.
Futuro Health CEO Van Ton-Quinlivan is a nationally recognized expert in workforce development. Her distinguished career spans the private, public and nonprofit sectors. She is a White House Champion of Change and California Steward Leader, and formerly served as Executive Vice Chancellor of the California Community Colleges.



